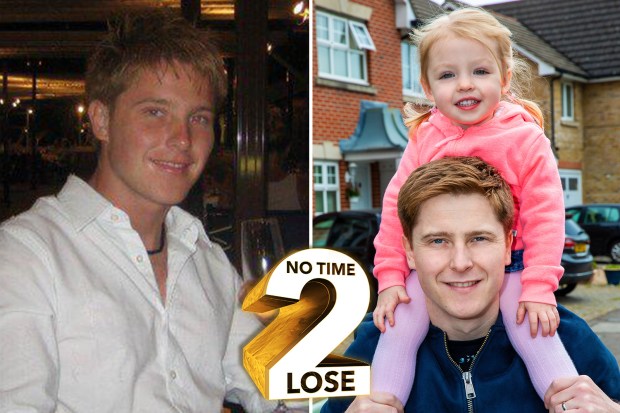
I got bowel cancer at 24 after doctors mistook it for trapped wind because I was so young
WAKING in the middle of the night in agony and drenched in sweat, Paul Simms felt like he was dying.
He had already been to the doctors twice about stomach pains and told it was probably just trapped wind.
But the 24-year-old, from Enfield, north London, knew it was more serious.
Over a period of a couple of weeks his weight had dropped and he had noticed blood in his poo.
Desperate for answers, Paul eventually saw a private doctor where his worst fears were confirmed - he had bowel cancer.
Not only that, but the tumour had attached itself to his bladder and pelvis, which would make the treatment even more complicated.
Paul, a branch manager for Travis Perkins, told the Sun Online: "Obviously it came as a shock, but at the same time it didn't.
"I knew something was seriously wrong because I felt bad for so long it didn't come as a surprise.
"It was almost a bit of a relief, because although it wasn't good news I knew it could now be dealt with."
He added: "On one hand, you could say I was let down. But then in the early stages, they're not going to think it would happen to someone that age."
Never too young
It comes as new research revealed the rates of bowel cancer in people aged between 20 and 29 have surged.
If the alarming trend continues, experts say the UK will have to screen at a lower age, to detect more cases at an earlier stage.
In England and Wales, everyone over the age of 60 is currently invited to have bowel cancer screening tests every two years. In Scotland screening starts at 50.
That's why The Sun launched the No Time 2 Lose campaign - to call on the Government to end the postcode lottery and lower the screening age to 50.
Bowel cancer is the second deadliest cancer in the UK, however, it can be cured if it's caught early enough through early diagnosis, which is why screening is so important.
Shooting pains
Paul, now 36, said he first started feeling unwell during a skiing trip with his friends in January 2008.
He recalled: "Everyone was having a good time and I didn't feel like joining in.
"A couple of weeks after getting back, I started getting shooting pains low down in my stomach, but I put it down to a bug or something.
"So I went to the doctor who said it was trapped wind and they gave me some medication.
"But my poos started getting thinner over a period of a couple of weeks, then all of a sudden I had this bad diarrhoea constantly, and there was blood in it as well.
"At that stage I kept going back to the doctor who said it was trapped wind, then they thought it might be IBS."
Paul says at this stage he asked to be referred to a specialist and got an appointment a few weeks later at University College Hospital in London.
But by this stage he was experiencing more symptoms.
He said: "I was losing weight and in quite a lot of pain. I just felt like I was dying.
"I was having night sweats - I was freezing cold all the time then I'd wake up in the night absolutely dripping covered in sweat. That was consistent.
"When I got to the appointment with the specialist, he did a physical examination and said it could be a number of things.
"He said they'd get me back in for a colonoscopy in six weeks' time.
"I went with my dad and when we came out I turned to him and said, 'I can't wait six weeks'. I knew something was seriously wrong."
He begged his parents to take him to see a private doctor and within a few days he was diagnosed with cancer.
From there he went back to the NHS for treatment, adding: "They were really good from then and everything developed really quickly."
Paul was sent for a CT and MRI scan and doctors saw that the tumour had grown to "quite a size" and attached itself to his bladder and pelvis.
He said: "It meant my treatment had to be slightly different - usually you would just operate by cutting a section of the bowel out and rejoining it.
"But because it was stuck to the bladder and pelvis what they did was give me a temporary ileostomy and opened me up to have a look at what they were dealing with."
I felt like I was dying and I was just in survival mode
Paul Simms
At the same time, he was told any further treatment could leave him infertile and he should consider storing some sperm.
He said: "I remember my mind was just blown. I was single at the time, so it was not a priority.
"There was a really good nurse and she sat me down and was like, 'I know you're not thinking about that at all, but you should'.
"My parents agreed so I reluctantly did it in the end - but it really wasn't something I felt like doing at the time.
"I felt like I was dying and I was just in survival mode.
"I guess I was a pretty immature 24-year-old, and if I didn't have the influences I did then I wouldn't have bothered."
The 6 ways you can prevent bowel cancer
IT'S the second deadliest cancer in the UK but it can be prevented.
A few simple lifestyle changes can help stop bowel cancer striking in the first place.
They are:
- Get screened - if you are eligible, don't delay, book your screening test as soon as you get the letter
- Stop smoking - around 8 per cent of bowel cancer cases are linked to smoking
- Cut back on the booze - sticking to the recommended 14 units a week, that's six pints or 10 small glasses of wine, reduces your risk
- Get moving - aim to do 30 minutes of exercise a day
- Eat well - up your fibre intake, it's vital to keep your bowels moving and there's evidence to suggest cutting back on red meat helps
- Drugs work - there's no magic pill, but there is evidence to suggest a daily dose of aspirin lowers the risk of polyps, a precursor to bowel cancer
Paul went on to have two rounds of chemotherapy and six weeks of chemo radiation to try and shrink the tumour enough so they could operate.
He said: "They said they didn't know how successful it was going to be and I had to wait another eight weeks to know if it was going to work.
"Scans showed it had shrunk from the size of a tennis ball to a golf ball so they got me in for an operation to remove it.
"A little bit later I went back and had the bag reversed, followed by another six months of chemo."
Fortunately, his treatment was a success - and has been cancer-free since.
Four years after getting the all-clear he met his now wife Kayleigh, 33, and was open with her about his likelihood of being able to conceive.
He said: "In the back of my mind I always hoped that everything would be fine.
“But then deep down, I knew that there would probably be a problem. It was difficult to face the reality that having a child may not happen.”
Paul added: “It was quite tough. I am a man with an ego and it’s really hard to face up to that kind of thing. There was a lot of pride there.
"I was quite good at blocking things out. Sometimes it’s the way I deal with things.
“I didn’t want to talk about it, even with my wife really to a certain extent, and certainly not with friends and family”.
After trying to conceive for a while without success, the couple, who were living in Stevenage, Herts, at the time, consulted with doctors and fertility specialists.
They were told that their chances of having a baby without assisted conception techniques would be slim.
NEVER TOO YOUNG
HISTORICALLY bowel cancer has been more common in the over 50s, but this new research suggests the tide may be turning.
Every year in the UK, 2,500 Brits under 50 are told they have the disease - the second most deadly cancer in the country.
Deborah Alsina, CEO of Bowel Cancer UK, said these figures show why it's so important to warn young people they too are at risk of bowel cancer.
"This is exactly why we launched our , which aims to stop young people dying of bowel cancer," she said.
"We can do that by improving clinical practice, increasing overall awareness and ensuring access to screening for those most at risk.
"The time has passed where it is in any way acceptable to tell someone under 50, who presents with symptoms, that they are 'too young for bowel cancer'."
The new studies show rates in the 50 to 74-age group have "significantly decreased" in some countries.
Ms Alsina said that is likely to be down to screening.
"While progress has been made in the UK, it is not significant," she warned.
For the Government to honour its pledge to lower the screening age to 50 in England, the NHS needs to roll out a new, more effective screening test.
The FIT test requires just one stool sample, rather than three - and pilot tests have proved people are much more likely to use it.
But, plans to roll out the new test have been repeatedly put on hold. It was due to be introduced last autumn, then that date was moved to April - yet there is still no sign of it.
Ms Alsina said it is vital the powers that be commit to a clear plan to roll out FIT and lower the screening age to 50 as soon as possible - a move that could save up to 4,500 lives every year.
She said: "Bowel cancer does not need to be the UK's second most deadly cancer, it can be cured - or better still, prevented.
"We need action now to recognise the changing nature of the disease and to put in place measures that enable the whole population to benefit from the opportunity of an early diagnosis when the disease is most treatable."
Paul said: “No one really knows how much chemotherapy and radiotherapy treatment affects sperm and how much and in what way.
"So even if we had conceived naturally there could have been all manner of complications further down the line."
The couple were told they were eligible for NHS-funded IVF treatment using the sperm Paul had frozen years before he met Kayleigh.
Paul said: “My dad dropped me off outside University College Hospital, where the sperm had been frozen, and I was handed a container of liquid nitrogen which looked like something pretty similar to what a security guard would collect cash in from a business or bank."
Fatherhood is the best thing I’ve ever done, and I’m grateful to be in this position now because for a time it didn’t feel like I would ever be a dad
Paul Simms
He then took the two hour journey to Bourn Hall clinic, just outside Cambridge, so it could be thawed in their lab.
Paul said: "It felt like a lifetime. I had to be careful, I kept thinking 'what if I crash or there is an accident?'"
Once in the lab, Paul's sperm was thawed and directly injected in to a number of Kayleigh’s harvested eggs using a process called Intracytoplasmic Sperm Injection (ICSI).
One of the resulting embryos was transferred to Kayleigh’s womb and the couple were delighted when they were told she was pregnant after her second treatment.
Daughter Sophie was born on July 31, 2016, and is now a lively, bubbly toddler.
NO TIME 2 LOSE
Paul's remaining frozen sperm remains stored at Bourn Hall and the couple say they have every intention of having further IVF treatment in the hope of having a brother or sister for Sophie.
He said: “We are definitely going back to Bourn Hall to try again as we definitely want another baby, in fact Kayleigh would like another two but we will have to see."
He added: “Fatherhood is the best thing I’ve ever done, and I’m grateful to be in this position now because for a time it didn’t feel like I would ever be a dad and have a child wishing me a Happy Father’s Day.”
We pay for your stories! Do you have a story for The Sun Online news team? Email us at tips@the-sun.co.uk or call 0207 782 4368 . You can WhatsApp us on 07810 791 502. We pay for videos too. Click here to upload yours.

















